
Mycosis of the foot (dermatophytosis) is an infectious disease caused by pathogenic or opportunistic fungi. During mycosis, the skin on the feet peels off and becomes very itchy, and in severe cases of the disease, it becomes red and swollen.
Definition of the disease
Mycosis of the foot, or dermatophytosis, is an infectious disease caused by a dermatophyte mold. In total, 43 types of dermatophytes are known, 30 of which cause foot mycosis. Most often these are fungi Trichophyton rubrum (90%), Trichophyton mentagrophytes and less often Epidermophyton. Fungi of the Candida genus and molds Scytalidium dimidiatum, Scytalidium hyalinum cause mycosis of the feet much less often.
All dermatophytes have keratinolytic activity: they can dissolve keratin, the fibrous protein that makes up the upper part of human and animal skin. The skin is damaged.
After getting on the skin, the fungi are directed to the most vulnerable places - to the junction between the cells of the epidermis. There they penetrate inside and start active growth. However, fungi rarely penetrate deeper than the granular layer of the skin. As a rule, they are limited only to the upper, keratinized tissues.
Spread of foot mycosis
Cutaneous mycoses, including foot mycoses, are found in all countries of the world. The share of these diseases in the structure of all dermatological diseases reaches 37-40%.
At the same time, mycoses of the skin occur most often - in about 30% of cases.
According to dermatologists, up to 20% of the adult population suffers from foot mycosis. Pathology occurs twice as often in men.
In people over the age of 70, foot fungus occurs in almost every second patient - this is explained by the fact that the elderly usually have chronic diseases associated with metabolic disorders, as well as vascular pathologies, such as varicose veins.
Infection with mycosis of the foot usually occurs in the family - through direct contact with the skin of an infected person. Cases of infection by sharing clothes, shoes and household items are also known.
The infection usually affects both feet at the same time and partially spreads to the nail plates. Without treatment, the disease can also affect the skin of the hand - usually the working hand. This condition is called two legs one hand syndrome.
Causes of foot mycosis
Most often, foot mycosis is caused by dermatophyte fungi - Trichophyton rubrum, Trichophyton mentagrophytes and Epidermophyton floccosum. Much less often, the disease is provoked by fungi of the genus Candida (Candida) and mold (Scytalidium dimidiatum, Scytalidium hyalinum).
According to some studies, the proportion of dermatophytes in the causative agents of foot mycosis is gradually decreasing. Candida fungus comes to the fore.
Risk factors for the development of foot mycosis:
- Violation of personal hygiene;
- sharing shoes (for example, in bowling alleys, skate and ski rental shops);
- visiting public baths, swimming pools, beaches;
- Climatic characteristics: the risk of illness is higher in countries with a subtropical and tropical climate - this is due to increased humidity and environmental temperature;
- constantly wore closed, tight shoes (this happens in military personnel, miners, textile and metallurgical industry workers);
- Frequent injuries of the toes due to flat feet, bunions, corns;
- non-compliance with sanitary rules during pedicure;
- violation of blood supply to the legs;
- immunodeficiency conditions, including HIV;
- chronic dermatoses;
- obesity;
- diabetes;
- chronic venous insufficiency;
- Taking certain medications (systemic glucocorticosteroids).

Symptoms of foot mycosis
The symptoms of mycosis of the feet, as well as the features of the treatment of the disease, depend on its clinical form.
Flat (flat-hyperkeratotic) form of foot mycosis
In most cases, the causative agent of the flat form of foot mycosis is the dermatophyte Trichophyton rubrum.
At the initial stage of the disease, the patient suffers from moderate peeling of the skin between the fingers - the scales on the skin are abundant, thin and silvery. Then, when the disease spreads to the lateral and dorsal surfaces of the legs, a characteristic inflammatory ridge appears and the skin thickens in the affected areas. Over time, the patient develops onychomycosis - nail fungus.
Intertriginous (interdigital) form of foot mycosis
This form often develops against the background of heavy sweating of the feet. The disease affects the spaces between the fingers and is accompanied by redness, swelling and maceration (softening and loosening of the skin). Erosion and cracks are often formed. Many patients report itching, burning and pain.
Simultaneous infection of the foot skin with dermatophytic fungi (usually Trichophyton mentagrophytes var. interdigitale) and Staphylococcus aureus bacteria often occurs.

Dyshidrotic form of foot mycosis
As a rule, the causative agent of this form of foot mycosis is Epidermophyton floccosum.
The dyshidrosis form of foot mycosis is usually more severe and is accompanied by painful itching and pain. Blisters with a thick coating form on the skin. As a result of fusion, they form large multi-chambered blisters, which, after opening, turn into moist pink-red erosions, and then into brown crusts.
The disease is difficult to treat and often recurs.
A characteristic feature of the dyshidrosis form is damage to the skin of the arch of the foot, interdigital folds and fingers. The process can then spread to the heels, the lower lateral surfaces of the feet, and even the skin below the ankles.
If a bacterial infection occurs, the patient may develop a fever and regional lymph nodes may become enlarged. Swelling of the leg appears and the skin on it becomes wet. Severe pain makes it difficult for the patient to walk.
Exudative-dyshidrosis form of foot mycosis
Most often, the exudative-dyshidrosis form of foot mycosis is caused by the fungus Trichophyton rubrum (red trichophyton).
First of all, the skin between the fingers is damaged. Then the process spreads to the sole of the foot, the dorsal and lateral surfaces and the nail plates. Blisters and erosion appear on the skin, which are then covered with a crust. The skin becomes moist and may ooze.

Deleted form of foot mycosis
A deleted form has been identified by some researchers. It is believed to occur a few days after being infected with the fungus.
The skin in the interdigital folds begins to peel. There may also be minor peeling on the feet and sides. Patients may ignore unpleasant symptoms, but still infect others.
Acute form of foot mycosis
The acute form of mycosis of the feet is the result of an exacerbation of the dyshidrosis or intertriginous (interdigital) form.
The disease begins acutely: a large number of blisters appear on the skin of the feet, and then on the legs. The skin is swollen. Then knots are formed on the hands and the lower third of the forearms.
After the blisters open, erosion appears, surrounded by loose skin debris. They merge, turning into wide weeping surfaces, often with purulent discharge.
The disease is often accompanied by fever, worsening of the patient's general condition and sharp pain in the affected hands and feet. The lymph nodes in the groin and thigh are enlarged and painful.
Vesiculobullous (inflammatory) form of foot mycosis
The inflammatory form of foot mycosis is usually identified by foreign authors, often defining it as acute. It can develop into a chronic interdigital form of dermatophytosis.
As a rule, the causative agent of the vesiculobular form is the dermatophyte Trichophyton rubrum.
Main symptoms: severe itching, skin rashes, localized mainly on the soles, the bottom of the fingers and on the sides, on the back of the foot. Swollen areas with blisters on the surface may appear. Bubbles can merge or remain unchanged for a long time - if the tire (top) is thick enough.
Often the nail plates are also involved in the process - onychomycosis develops.
Ulcerative form of foot mycosis
The ulcerative form (in foreign literature it is called deep) is one of the complications of mycosis of the foot, which is caused by the addition of bacterial infection.
Wide deep purulent ulcers form on the soles. The patient experiences severe pain and, as a result, has difficulty walking.
Complications of foot mycosis
Cracks and sores on the skin that appear at the site of mycosis are the gateway to bacterial infections. However, such infections are more difficult to treat – this is explained by the fact that fungi produce special substances that increase the resistance of bacteria to drugs.
The most common complications of foot mycosis:
- infectious and drug-induced allergic dermatitis;
- Pyoderma - pustular skin diseases (cellulitis, lymphangitis, phlegmon, osteomyelitis of the leg bones), which can cause deep, long-lasting skin wounds;
- plantar warts;
- Microbial eczema is a chronic inflammatory disease in which the skin itches and reddens, and blisters of liquid form appear on it;
- general decrease of immunity and microcirculation disorder in the lower limbs (usually develops in patients with diabetes and varicose veins);
- spread of the disease on the skin of the hands and nail plates;
- Deterioration of quality of life: in acute forms of mycosis, it is difficult to wear shoes, and lymphadenitis causes fever and deterioration of health.

Diagnosis of foot mycosis
A dermatologist-mycologist deals with diagnosis and treatment of foot mycosis.
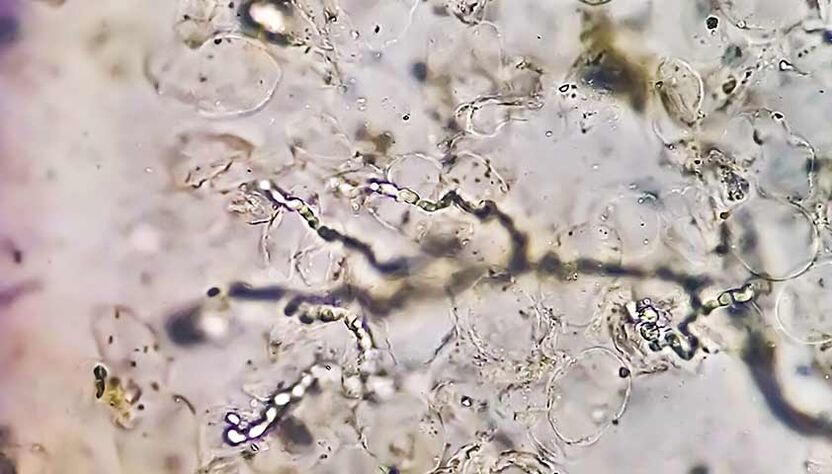
During the appointment, the doctor will assess the condition of the patient's nails, skin, mucous membranes and hair. He will perform a dermatoscopy - examine the skin under magnification. Along with the examination, the specialist will collect an anamnesis and ask the patient about his lifestyle, quality of food, household habits and care procedures.
If you suspect athlete's foot, your doctor will order lab tests.
Examination of skin scrapings can rule out or confirm a fungal infection.
The doctor may also refer the patient for microscopic examination and culture.
Sowing, i. e. the cultural method, allows you to get more accurate information about the causative agent of the disease, although it takes more time - usually a month.
Diabetes can significantly worsen the course of foot mycosis and cause serious complications. Complex studies can exclude or confirm this diagnosis.
A complete blood count helps to assess the patient's general condition.
A clinical blood test is a blood test that allows you to evaluate your general health, identify inflammation, bacterial, viral and fungal infections, and also help in the diagnosis of anemia, diseases of the hematopoietic organs, allergic reactions and autoimmune diseases.
Also, before recommending antifungal therapy, the doctor may prescribe a biochemical blood test to the patient - this study determines the level of bilirubin and liver enzymes ALT and AST. Such information will help the doctor to select the dose of the drug and minimize the risk of side effects.
Treatment of foot mycosis
Treatment of foot mycosis is carried out in two stages.
On the first stageIn case of acute inflammation, lotions are used: aqueous solution of ammonium bituminous sulfonate, agents with antiseptic properties (Castellani liquid, brilliant green 1% aqueous solution). Then pastes and ointments containing antifungal and glucocorticosteroid drugs are prescribed.
Anti-inflammatory solutions in the form of lotions, as well as combined antibacterial agents in the form of creams and solutions, are used during severe crying (in the acute phase) and secondary infection.
The basis of therapy is the use of antimycotic - antifungal agents.
at the main stageIn the treatment, antifungal agents are used, which are designed to destroy pathogenic fungi. Most often, such medicines are produced in the form of ointments, creams or solutions.
If the patient suffers from severe itching, the dermatologist may prescribe antihistamines. They are usually taken for 10-15 days until the unpleasant symptom disappears completely.
When nails are damaged, antifungal agents are used - they are applied directly to the nail plate and nail folds. In this case, the drug concentrates on the surface of the nail and does not reach the blood, which eliminates the risk of side effects.
If external drugs do not give an effect, systemic antimycotic drugs are prescribed.
The doctor determines the treatment regimen and dosage of drugs. During the treatment period, it is necessary to visit the pediatrician at least once a month.
Prognosis and prevention
If you consult a doctor in time, the prognosis of mycosis of the foot is favorable: most patients treated with antifungal drugs get rid of the disease forever.
To prevent mycosis, you should protect your feet and hands from irritating and traumatic factors and strengthen your immune system.
Onychomycosis prevention measures:
- Change your socks every day or more often if your feet are sweaty or wet;
- Air or dry shoes after wearing;
- Use an anti-fungal UV shoe dryer;
- Do not wear common slippers when visiting;
- Do not try on shoes in the store with bare feet;
- Use a personal towel for your feet;
- use individual nail care tools (tweezers, files);
- wear shoes in the pool or sauna;
- control the diversity of your diet;
- Avoid stressful situations.
FAQ
How to treat foot fungus?
Antimycotic agents are commonly used to treat foot fungus, which are available in the form of creams, ointments, and solutions. A dermatologist should choose the most effective drug and determine its dosage.
why do my feet hurt
One of the causes of itchy feet is athlete's foot, an infectious disease caused by a dermatophyte mold.



























